Atherosclerosis obliterans (ASO), especially of the lower extremities, is associated with a spectrum of cutaneous findings, ranging from slowly progressive ischemic changes to the sudden appearance of ischemic lesions following atheroembolization. Atheroembolism is the phenomenon of dislodgement of atheromatous debris from an affected artery or aneurysm with centrifugal microembolization and resultant ischemic and infarctive cutaneous lesions.
Causes
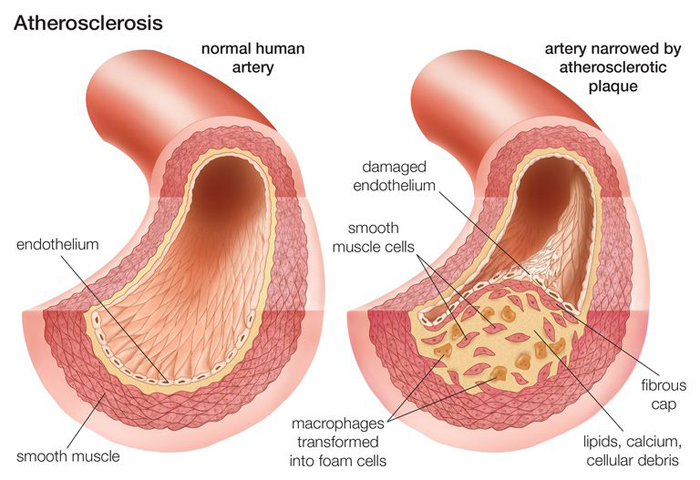
Atherosclerosis is the most common cause of arterial insufficiency and may be generalized or localized to the coronary arteries, aortic arch vessels to the head and neck, or those supplying the lower extremities, i.e., femoral, popliteal, anterior and posterior tibial arteries. Atheromatous narrowing of arteries supplying the upper extremities is much less common. Atheromatous deposits and thromboses occur commonly in the femoral artery in Hunter’s canal and in the popliteal artery just above the knee joint. The posterior tibial artery is most often occluded where it rounds the internal malleolus, the anterior tibial artery where it is superficial and becomes the dorsalis pedis artery. Atheromatous material in the abdominal or iliac arteries also can diminish blood flow to the lower extremities as well as break off and embolize (atheroembolization) downstream to the lower extremities. Detection of atherosclerosis is often delayed until an ischemic event occurs, related to critical decrease in blood flow.
In addition to large-vessel arterial obstruction, individuals with diabetes mellitus often have microvasculopathy associated with endothelial cell proliferation and basement membrane thickening of arterioles, venules, and capillaries.
Atheroembolism Multiple small deposits of fibrin, platelet, and cholesterol debris embolize from proximal atherosclerotic lesions or aneurysmal sites. Occurs spontaneously or after intravascular surgery or procedures such as arteriography, fibrinolysis, or anticoagulation. Emboli tend to lodge in small vessels of skin and muscle and usually do not occlude large vessels.
Symptoms
Symptoms of atherosclerosis are usually not seen until blood flow becomes slowed or blocked. Typical symptoms of atherosclerosis include chest pain if an artery to the heart is involved. or leg pain when a leg artery is involved. Sometimes symptoms occur only with activity. In some people, however, they may occur at rest.
Symptoms you may have depend on which arteries are severely narrowed or blocked.
- If the arteries that feed your heart (coronary arteries) are affected, you have symptoms of coronary artery disease.
- If the arteries that feed your legs, pelvis, or arms are affected, you have symptoms of peripheral arterial disease.
- If the arteries that feed your kidneys are affected, you have symptoms of renovascular hypertension.
Diagnosis
Clinical suspicion confirmed by arteriography and deep skin biopsy (atheroembolism). To make a diagnosis, your doctor will:
- Ask about your health history and risk factors
- Ask about your family history of atherosclerosis or its complications
The physical exam may include:
- Listening to your arteries for an abnormal whooshing sound, called a bruit. A bruit can be heard with a stethoscope when placed over the affected artery.
- Checking to see if any of your pulses (for example, in the leg or foot) are weak or absent.
Treatment
Diet First step in management of primary hyperlipidemia: Reduce intake of saturated fats and cholesterol as well as calories.
Exercise Useful adjunct to diet. Walking increases new collateral vessels in ischemic muscle.
Hypertension Reduce elevated blood pressure
Cigarette Smoking Discontinue.
Blood Correct anemia or polycythemia.
Positioning of Ischemic Foot As low as possible without edema.
Drug Therapy Recommended for adults with LDL cholesterol > 190 mg/dL or > 160 mg/dL in the presence of two or more risk factors after an adequate trial of at least 3 months of diet therapy alone. Initiation of drug therapy usually commits patients to lifelong treatment. Drugs act primarily by lowering LDL cholesterol and include bile acid-binding resins, nicotinic acid, and HMG-CoA reductase inhibitors.
Intermittent Claudication
Medical Management Encourage walking to create new collateral vessels.
Surgical Management Endarterectomy or bypass for aortic iliac occlusions and for extensive femoral popliteal disease.
Ischemia/Infarction of Foot/Leg
Surgical Management Distal bypass surgery of three crural arteries.
Atheroembolization Response to surgical revascularization or thrombolytic therapy often poor.
Medical Management Heparin and warfarin. Analgesics.
Surgical Management Debridement of necrotic tissue locally or amputation if indicated. Remove or bypass atherosclerotic vessel or aneurysm. Amputation of leg/foot: indicated when medical and surgical management has failed.
Prevention
Goal of management is prevention of atherosclerosis rather than treatment of ischemic complications.
References