Definition
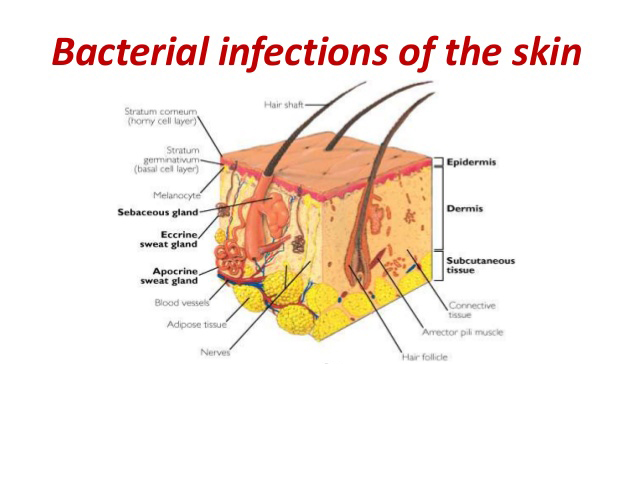
Invasion of the skin, its appendages, and/or subcutaneous layer by way of thermal, mechanical, chemical, or physiologic injury and the colonization or infection with pathogenic bacteria of both aerobe and anaerobic nature. Lesions are usually due to immune system response and purulence is present.
Classified as follows: Boils and abscesses: Localized-isolated skin soft tissue collections of infection.
Furuncles, carbuncles: Local infections of hair follicles single and multiple respectively.
Folliculitis: Local or widespread areas of multiple small distal infections of pilosebaceous units.
Impetigo: Superficial epidermal infection (Staphylococcus aureus and Streptococcus pyogenes are the most common skin pathogens). Ecthyma: Deep epidermal and high dermal infection with same staphylococcal streptococcal bacteria.
Erysipelas, cellulitis: Infection of deep skin layers into subcutaneous layer; widespread and diffuse.
History
Symptoms Boils and abscesses: Small and large, localized, tender, painful, red, and inflamed.
Furuncles, carbuncles: Single or several single in confluent group of red papules, wann and tender.
Impetigo: Weepy, crusty sores, single or multiple, small and large. Some tenderness, rare fever.
Ecthyma: Large weepy crusty almost ulcerative sores; occasional fever and tenderness.
Erysipelas, cellulitis: Red, warm, swollen, tender, and painful skin areas. Fevers common. Eye may be swollen closed.
General: Investigate environmental exposures or known contacts for skin injury and bacterial proximity.
Age
Boils, abscesses: Any, but usually more prevalent post pubescent.
Furuncles,carbuncles: Any, but more common in teens and adults.
Folliculitis: Any.
Impetigo: Any, but more common in children.
Ecthyma: Any.
Erysipelas, cellulitis: Any, but usually in the adult.
Onset
Boils, abscesses: Suddenly, with small surface papule or deeper indurated small nodule.
Furuncles, carbuncles: Sudden with chronic spread possible from single to several lesions.
Folliculitis: Sudden with few to many lesions, to chronic beginning few local to widespread many areas.
Impetigo: Sudden with one or more papules.
Ecthyma: Sudden with one or more lesions.
Erysipelas, cellulitis: Sudden but insidious.
Duration
Boils, abscesses: Days, weeks, or months until treated.
Furuncles, carbuncles: Days, weeks, or months until treated.
Folliculitis: Weeks, months, or years until treated. Impetigo: Weeks or months unless treated.
Ecthyma: Weeks or months .
Erysipelas, cellulitis: Weeks, and can have serious complications if untreated.
Intensity Boils, abscesses: Single to few, almost asymptomatic to widespread with systemic signs (e.g., fever, listlessness).
Furuncles, carbuncles: Few local to many widespread with only minimal systemic potential.
Folliculitis: Small, local to extensive widespread. Rare systemic effect.
Impetigo: Single to multiple and widespread lesions with systemic effect possible in extensive disease.
Ecthyma: Single to multiple and widespread lesions with systemic effect possible in extensive disease.
Erysipelas, cellulitis: Mild to extensive local lesions with mild to severe systemic signs common.
Aggravating Factors: Further or continued exposure to skin traumatizers, lack of treatment, uncleanliness, poor hygiene, immune deficiency.
Alleviating Factors: Meticulous, gentle skin cleansing especially with antibacterials, strong efficient immune system.
Associated Factors: Environmental exposure.
Physical Examination
General: The patient usually appears in no acute distress. Obtain temperature and vital signs to evaluate for the possibility of sepsis.
Skin
Boils and abscesses: Papular or nodular soft tissue indurations with inflammation and tenderness. Abscesses will be fluctuant at some time in their course and may exhibit a point with a purulent top. May be in any soft tissue location, but most common in the axillae, groin, and high inner thighs. Any skin gland, node, or opening can develop an abscess.
Furuncles, carbuncles: Found everywhere there are sweat or oil ducts, but most common upper back, chest, neck, axillae, and groin. Inflammed, single pustules seen with furuncles and groups of small neighboring pustules in single inflammed lesion seen with carbuncles. Carbuncles may be quite tender.
Folliculitis: Single, red papules and/or pustules scattered diffusely and widely over the body anywhere there are hair follicles. May be seen in smaller local groups or patches (e.g., the whisker area, buttocks, or chest). Usually no surrounding erythema or inflammation.
Impetigo: Small red papules, vesicles, or pustules seen initially. May develop into roundish, broad, superficial, crusted weepy erosions. Thick-piled crusts of honey-brown are generally due to Streptococcus and thin smooth crusts due to Staphylococcus. Lesions may be solitary or multiple and exist in a wide area or grouped closely. Generally on the face of children, but may affect any location.
Ecthyma: Slightly inflammed deeper erosions with moist or dry crustingin concentric lesions of skin. May occur in any location, usually on smooth skin.
Erysipelas, cellulitis: Local marked erythematous swellings with discreet, raised border and mild honey weep. Seen on dry warm surface of facial areas (e.g., ear, cheeks, nose, periorbital area in adults). Local large or small erythematous warm, tender, irregularly bordered swellings of skin and soft tissues in any area of the child or adult. Often associated with fever and listlessness. May have moist serous ooze on surface with cellulitis.
Lymphatic: All of the bacterial skin infections may cause local or regional lymph node swelling and tenderness.
Pathophysiology
S. pyogenes, and S. aureus (nonresident flora) are the most common bacterial skin pathogens although sometimes caused by resident bacteria as diphtheroids and coagulase negative staphylococci. Haemophilus injfuenzae may be the cause of childhood facial cellulitis.
Pseudomonas aeruginosa is encountered in some whirlpool, hot tub, swimming pool folliculitis. S. epidermidis may be the causative agent in some body abscesses.
Occasional anaerobes of abscesses are peptococci, and propionibacterium species. Perineal, genital, buttock abscesses often contain fecal bacteria (e.g., alpha and nonhemolytic streptococcus, anaerobic gram-positive cocci, and bacteroides species).
Diagnostic Studies
Usually none needed but on occasion used to differentiate pathogen especially if systemic signs and symptoms are present.
Laboratory
Culture with Gram stain: Of the lesion to identify the causative organism.
Complete blood count: May show an elevated white blood cell count with systemic infections.
Differential Diagnosis
Traumatic
Wounds: Especially those of the puncture or penetrating type, may lead to infections with less common, more difficult bacteria, (e.g., Tetanus welchi, P. aeruginosa, etc.) which require specialized antibiotic treatment or tetanus innoculation.
Infectious
Fungal kerions: Can mimic boils, abscesses, furuncles, or carbuncles and may even be colonized with double infection. Usually less inflammation with lesions solely due to fungal organisms, but only culturing will differentiate. Most common on scalp.
Folliculitis (Fungus and chemical): Including steroids, (e.g., cortisones, androgens). Differentiated by resistance to treatment, potassium hydroxide (KOH) preparations, Gram stains, and/or cultures of intrafollicular matter.
Pityrosporum orbiculare: Most common fungal/yeast pathogen. Occasional P. aeruginosa seen with a history of frequent whirlpool or hot tub use.
Herpes virus: In crusted ulcer stage can look like impetigo, but recurrent history, location, and prodrome are different.
Tularemia: is a gram-negative bacillus disease from Francisella tularensis causing ecthyma like ulcers. Usually seen on the arms and hands of rabbit handlers. May occur anywhere on the body if due to tick borne disease.
Ulcers: Few, just at site of skin entry. Respond to streptomycin or gentamycin.
Metabolic: Not applicable.
Neoplastic
Some basal, squamous cell cancer, and metastatic lesions to the skin: May appear as furuncles, carbuncles, abscesses, or ulcerations. Their chronic non tender sterile nature differentiates.
Vascular: Not applicable.
Congenital: Not applicable.
Acquired: Not applicable.
Treatment
Boils and Abscesses: Uncomplicated with no cellulitis: Usually heal after sterile incision and drainage accomplished with sterile #11 blade and local anesthetic or Frigiderm topical freeze anesthesia. If ripe pustular point is present, no anesthesia may be required. Hot compresses may be applied 15 to 30 minutes 2 to 3 times daily until the lesion dries out. This is performed if there is no drainage and the lesion is healed closed. If large, (greater than 2 cm) a gauze or rubber drain may facilitate healing. Remove after 3 to 5 days. If complicated by number of lesions or gangrene, or serious host immunodeficiency or cellulitis systemic disease signs, then systemic antibiotics may be needed after Gram stain and culture.
Antibiotic therapy consists of: Dicloxacillin 250 mg four times a day for adults, or erythromycin 250 to 500 four times a day for 10 days (Adults, under 60 lbs. 125 mg four times a day), or azithromycin 250 mg 2 capsules together day one then one daily for 4 days, or ceclor 500 mg twice a day. Clindamycin in recommended doses is an alternative in penicillin or cephalosporin allergic patients.
Furuncles and carbuncles: For a small number of lesions, moist heat and/or incision and drainage usually is curative. If the lesions are widespread or there is significant surrounding inflammation cellulitis, use systemic antibiotics as listed above for abscesses.
Folliculitis: Tetracycline 250 mg one four times a day or two twice a day up to 6 weeks and longer. Erythromycin 250 mg four times a day or two twice a day up to 6 weeks and longer. Avoid hot tubs if suspected as a cause, stop oil contact and chronic friction (e.g., tight clothes).Other antistaphylococus antibiotics may be used.
Impetigo: If there are less than 3 lesions, small, treat with topical mupirocin, bacitracin, or other topical antibiotic preparations.
Dicloxacillin 250 mg four times a day best for thick or thin crusting or bullous lesions caused by Staphylococcus and/or Streptococcus.
Erythromycin 250 to 500 mg four times a day for first line therapy or in those who are penicillin-allergic.Clindamycin 150 mg four times a day or a cepholosporin (e.g., Cefalexin 250 mg four times a day) may be used as an alternative. All antibiotics are given for 7 to 14 days.
Ecthyma: Dicloxacillin, erythromycin, clindamycin, or cephalosporin as dosed for impetigo above.
Erysipelas and cellulitis: Penicillin V 250 to 500 mg four times a day 10 days or Bicillin CR 2 ml intramuscularly for adult or erythromycin 250 to 500 mg four times a day for 10 days or clindamycin 150 mg four times a day for 10 days or a first generation cephalosporin equivalent to cephalexin 250 to 500 mg four times a day for 10 days.
Obstetrical Considerations
Sulfonamides, erythromycin, and ciprofloxacin should be used with caution. Tetracycline is contraindicated.
References