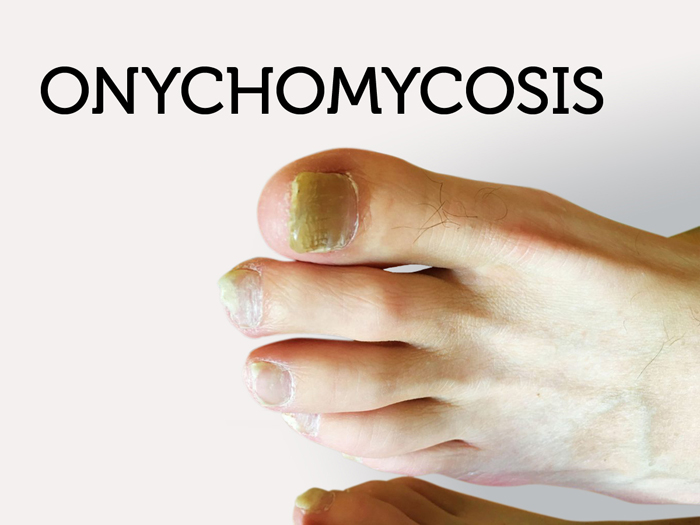
Onychomycosis is a chronic progressive infection of the nail apparatus, caused by dermatophytes most commonly, and less often by Candida sp. and molds. Tinea unguium refers to onychomycosis caused by the dermatophytes. Trichophyton rubrum has been imported into industrialized nations during the last century, resulting in an epidemic of onychomycosis, tinea pedis, and other types of epidermal onychomycosis. In addition to appearance, onychomycosis of toenails can cause pain, predispose to secondary bacterial infections, and ulcerations of underling nail bed. These complications occur more commonly in the growing population of immunocompromised individuals and diabetics.
Causes of Onychomycosis
Primary Onychomycosis Invasion occurs in an otherwise healthy nail. The probability of nail invasion by fungi increases with defective vascular supply (i.e., with increasing age, CVI, peripheral arterial disease), in posttraumatic states (lower leg fractures), or disturbance of innervation (e.g., injury to brachial plexus, trauma of spine).
Secondary Onychomycosis Infection occurs in an already altered nail, such as psoriatic or traumatized nail. Toenail onychomycosis usually occurs after tinea pedis; fingernail involvement is usually secondary to tinea manuum, tinea corporis, or tinea capitis. Infection of the first and fifth toenails probably occurs secondary to damage to these nails by footwear.
DLSO The nail bed produces soft keratin stimulated by fungal infection that accumulates under the nail plate, thereby raising it, a change that clinically gives the involved nail an altered cream color rather than the normal transparent appearance. The dense keratin of the nail plate is not involved primarily. The accumulated subungual keratin promotes further fungal growth and keratin production. The nail matrix is usually not invaded, and production of normal nail plate remains unimpaired despite fungal infection. In time, dermatophytes create air-containing tunnels within the nail plate; where the network is sufficiently dense, the nail is opaque. Often the invasion follows the longitudinal ridges of the nail bed. The subungual location of the infection could block effective topical antifungal agents.
Symptoms of Onychomycosis
Onychomycosis can be present for years without causing pain or disturbing symptoms. Typically, the nail becomes thicker and changes to a yellowish-brown. Foul smelling debris may collect under the nail. The infection can spread to the surrounding nails and even the skin.
Diagnosis
Clinical findings confirmed by finding fungal forms in KOH preparation and/or isolation of pathogenic fungus on culture.
Treatment
Indications for Systemic Therapy Fingernail involvement, limitation of function, pain (thickened great toenails with pressure on nail bed, ingrowing toe nails), physical disability, potential for secondary bacterial infection, Source of recurrent epidermal dermatophytosis, quality of life issues (poorer perceptions of general and mental health, social functioning, physical appearance, difficulty in trimming nails, discomfort in wearing shoes). Early onychomycosis easier to cure in younger, healthier individuals than in older individuals with more extensive involvement and associated medical conditions. It is essential to prove (fungal) infection before starting systemic treatment.
Debridement Dystrophic nails should be trimmed. In DLSO, the nail and the hyperkeratotic nail bed should be removed with nail clippers. In SWO, the abnormal nail can be debrided with a curette.
Topical agents Available as lotions and lacquer. Usually not effective except for early DLSO and SWO after prolonged use (months).
Amorolfine nail lacquer: reported to be effective when applied >12 months (available in Europe). Penlac: monthly professional nail debridement recommended.
Systemic agents Note: In systemic treatment of onychomycosis, nails usually do not appear normal after the treatment times recommended because of slow growth of nail. If cultures and KOH preparations are negative after these time periods, medication can nonetheless be stopped and nails will usually regrow normally.
Secondary prophylaxis Recommended for all patients. The entirety of both feet should be treated. Prophylaxis should be simple to use and inexpensive:
- Benzoyl peroxide soap for washing feet when bathing
- Antifungal cream daily
- Miconazole lotion/powder on feet
- Antifungal sprays or powders in shoes.
- Discard old, moldy shoes
- Pedicures/manicures: make sure instruments are sterilized or individuals have their own.
Prevention
Advice given is to keep the nails cut short and filed; to avoid trauma or irritations to the nails; to keep them cool and dry; and to wear good shoes that are not too tight or narrow.
References