Candidiasis of the oropharyngeal mucosa (OPC) occurs with minor variations of host factors as antibiotic therapy, glucocorticoid therapy (topical or systemic), age (very young, very old) as well as with significant immunocompromise. Esophageal and/or tracheobronchial candidiasis may be associated with oropharyngeal candidiasis and always occurs in the setting of advanced immunocompromise. Candida can invade through eroded mucosa, with resultant fungemia and invasive candidiasis.
Causes of Oropharyngeal Candidiasis
Most cases of Oropharyngeal Candidiasis are caused by the person’s own Candida organisms which normally live in the mouth or digestive tract. A person has symptoms when overgrowth of Candida organisms occurs.
It occurs more frequently and more severely in people with weakened immune systems, particularly in persons with AIDS.
Symptoms of Oropharyngeal Candidiasis
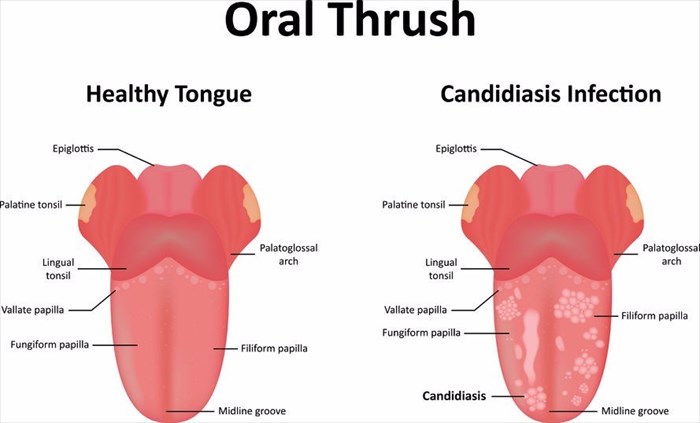
People with Oropharyngeal Candidiasis infection usually have painless, white patches in the mouth. Symptoms of OPC in the esophagus may include pain and difficulty swallowing.
Diagnosis
Clinical suspicion confirmed by KOH preparation of scraping from mucosal surface.
Treatment
Topical Therapy These preparations are effective in the immunocompetent individual but relatively ineffective with decreasing cellmediated immunity.
Nystatin Oral tablets, 100,000 units qid dissolved slowly in the mouth, are the most effective preparation. The oral suspension, 1 to 2 teaspoons, held in mouth for 5 min and then swallowed may be effective.
Clotrimazole Oral tablets (troche), 10 mg, one tablet 5 times daily may be effective.
HIV Disease Responds to topical and/or systemic therapy; however, recurrence is the rule, May become refractory to intermittent therapy, requiring daily chemoprophylaxis, with either topical or systemic treatment. Increase dose with resistant disease.
Fluconazole 200 mg PO once followed by 100 mg/d for 2 to 3 weeks, then discontinue. Increase the dose to 400 to 800 mg in resistant infection. Also available in IV form.
Itraconazole Capsules or oral solution. 100 mg PO qd or bid for 2 weeks. Increase dose with resistant disease.
Ketoconazole 200 mg PO qd to bid for 1 to 2 weeks.
Fluconazole-Resistant Candidiasis Defined as clinical persistence of infection after treatment with fluconazole, 100 mg/d PO for 7 days.
References